
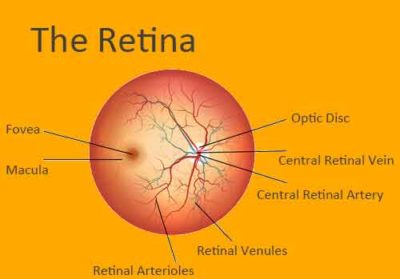
Diagnosis and classification ĭiabetic retinopathy is typically diagnosed by retinal exam observations using ophthalmoscopy. The repeated processes of blood vessel growth, swelling, and scarring can eventually cause retinal detachment, which manifests as the sudden appearance of dark floating spots, flashes of light, or blurred vision. Macular edema is the most common cause of vision loss in people with diabetic retinopathy. Left untreated, around 30% of those with such swelling experience vision disruption over the next 3–5 years. If the swelling occurs near the center of the macula, it can cause vision disruptions ranging from mildly blurred vision to severe loss of the center of an affected person's visual field. Īround half of people with diabetic retinopathy develop swelling of the macula, called macular edema, which can begin at any time. Minor bleeding can cause dark floating spots obstructing vision major bleeding can completely block vision. These new blood vessels often break and bleed. Eventually, many progress to a stage where new blood vessels grow throughout the retina. Then larger abnormalities in retinal vessels: cotton wool spots, hemorrhages, lipid deposits called "hard exudates", intraretinal microvascular abnormalities, and abnormal-looking retinal veins. Over time, progressive retinal damage may appear on a retinal exam, first with small bulges in retinal blood vessels called microaneurysms. For many, that damage can only be detected by a retinal exam, and has no noticeable effect on vision. Nearly all people with diabetes develop some degree of retina damage ("retinopathy") over several decades with the disease. Signs and symptoms Proleferative diabetic retinopathy Emptied retinal venules due to arterial branch occlusion in diabetic retinopathy (fluorescein angiography) It is also the leading cause of blindness in people aged 20 to 64. Each year in the United States, diabetic retinopathy accounts for 12% of all new cases of blindness. The longer a person has diabetes, the higher his or her chances of developing diabetic retinopathy.

In at least 90% of new cases, progression to more aggressive forms of sight threatening retinopathy and maculopathy could be reduced with proper treatment and monitoring of the eyes. It is a leading cause of blindness in developed countries.ĭiabetic retinopathy affects up to 80 percent of those who have had both type 1 and type 2 diabetes for 20 years or more. Nearly all patients with type 1 diabetes and >60% of patients with type 2 diabetes ĭiabetic retinopathy (also known as diabetic eye disease), is a medical condition in which damage occurs to the retina due to diabetes mellitus. Long-term poor control of diabetes mellitusĭiabetes, poor control of blood sugar, smoking Vitreous hemorrhage, Retinal detachment, Glaucoma, Blindness Often asymptomatic, but can cause spots in the eye and vision loss.


 0 kommentar(er)
0 kommentar(er)
